“I’m noticing a change in Renee.” These were the words from the lips of a capable in-home care partner (Jackie) when she was speaking with one of our dementia coaches about her client’s progress. Her client (Renee) is a wonderful lady, who is in the advanced stage of frontal-temporal dementia (FTD) and was manifesting very challenging behaviors that are often common during this stage.
For a moment, I was caught up in the excitement of how we are improving a person with dementia. Then, I was quickly brought back to reality, knowing that people with dementia do not improve in their condition. Alzheimer’s and related dementias (in this case FTD) progress in severity and there is no cure.
The reality of this “change” was not in Renee, but in Jackie. Her approach and the consistent use of effective strategies of care was changing Renee’s reaction to the care she was receiving. Renee’s quality of life was improving, but not the disease. This may seem to you to be semantics, but it is not. Renee’s condition will never change, but the symptoms can be managed effectively. When this happens, it looks like improvement. However, it is not a reversal of the disease but more an improvement in symptomatic outcomes.
So, what was the specific change in Renee and how was it accomplished? Renee was verbally and physically abusive in response to the efforts of caregivers. She was resistant to most care as well as walking and eating. With the help of our dementia Coach, Donna Sangi-Vallario, Jackie began to develop a new approach in communicating with Renee based on our Interactive Dementia Model (IDM).
Essentially, this model encourages the care partner to employ eye contact, appropriate body alignment, identification, frontal approach, validation of feelings, and several other strategies of care associated with IDM.
As I’m sure you realize by now, the primary change agent was Jackie. Like most of us, Jackie used strategies of care based on her understanding of life and how things “should be.” This is the mistake we all make in caring for someone with cognitive impairment. We ty to establish an environment according to our frame of reference. Using this approach in caring for someone diagnosed with dementia is the primary cause of problematic behaviors.
We need to step back and use the tools available to us. We get frustrated when the person is not responding to our definition of rationality. And, of course, anyone not responding to our conception of rationality is automatically irrational.
For example, a young child of 4 or 5 years of age would try to eat a quart of ice cream before dinner and not think anything wrong with this. Adults, of course, would be appalled at the thought. So, when the child exclaims, “why can’t I?” we immediately turn to what we know is correct and appropriate behavior and are able to give rational reasons for not engaging in the behavior. The child will obey you but will likely be disappointed. For the child, it makes all the sense in the world to eat a large bowl of ice cream, at any time.
The child does not yet have a developed sense of rationality like an adult. Nonetheless, the child is a rational human being. It is the job of the parent to help the child develop mature rationale. This can be a long and arduous task.
However, a person with dementia already has a mature rational mind, even though it may appear he/she does not. So, we may attempt to help them develop or re-develop this status of rationale. This will not work because the cause of challenging behaviors in not a symptom of irrationality. The person with dementia has every bit as much rationality as you and me, perhaps more given their longevity of life. The problem is identifying the correct frame of reference. The person with dementia has a different frame of reference than the one you think she/he should have. We need, as care partners, to discover the person’s frame of reference and approach accordingly.
While you may have clinical evidence of the person’s state of dementia, the person with dementia rejects such a proposition, especially those who are mid to late stage. When you change your approach to accommodate the person’s frame of reference you will begin to see a “change” as Jackie experienced. It looks like recovery but it really is just harmony of mindset.
We have witnessed incredible changes in symptomatic outcomes over the years. We have also seen family members and professional care partners alike become stunned when they experience these dramatic changes.
Whether the care partner is a spouse, a daughter, a son or an in-home aide or nurse, social worker or some other professional, we must all learn to adopt an approach commensurate with the person’s frame of reference.
Fortunately for Renee, Jackie is a good fit in caring for someone with dementia. Sadly, this is not the case with every caregiver. The goal in finding proper care is finding someone who can change his/her mindset quickly or has the potential to do so. We have trained thousands of caregivers in best practices dementia care. There are many with the potential to change mindset according to the person’s frame of reference to meet the needs of this precious segment of the elderly population. Find them – they’re out there. We see them all the time.






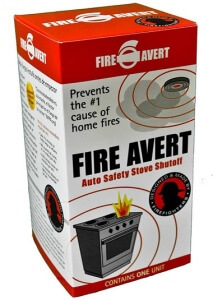 More good news…because Peter loves the idea of his product helping the likes of his grandma and mom to keep on making his favorite pies, he is generously giving those who love people with dementia a 20% discount off Fire Avert. If you’re interested, please visit
More good news…because Peter loves the idea of his product helping the likes of his grandma and mom to keep on making his favorite pies, he is generously giving those who love people with dementia a 20% discount off Fire Avert. If you’re interested, please visit 



